Overview of Autonomic Pharmacology
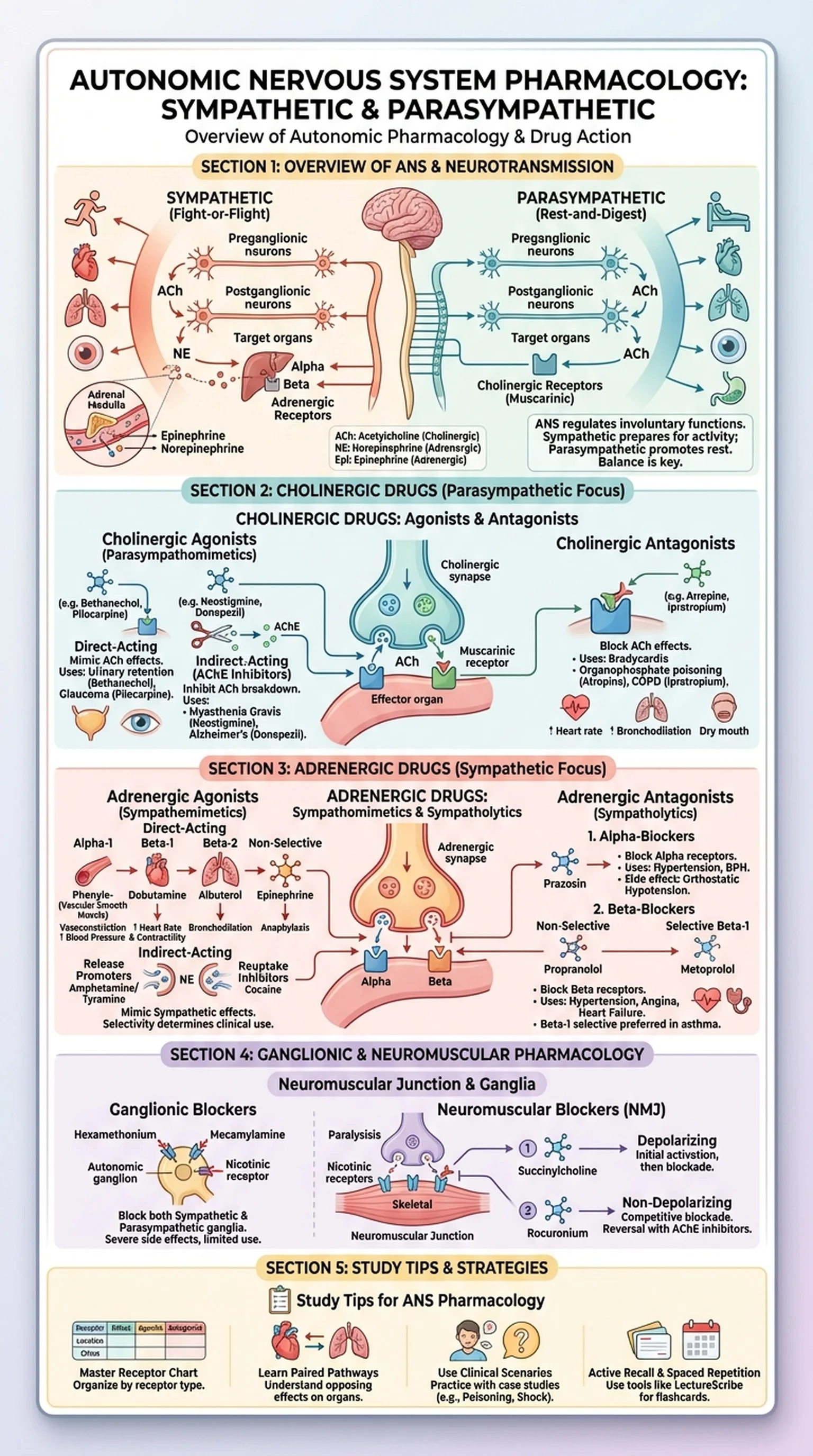
Autonomic pharmacology is the study of drugs that modulate the autonomic nervous system (ANS), the division of the nervous system responsible for regulating involuntary physiological processes such as heart rate, blood pressure, digestion, and glandular secretion. The ANS operates largely below conscious awareness and is divided into two major branches: the sympathetic nervous system and the parasympathetic nervous system. Understanding how sympathetic drugs and parasympathetic drugs influence these branches is essential for treating a vast array of clinical conditions.
The sympathetic nervous system mediates the fight-or-flight response, preparing the body for physical activity by increasing heart rate, dilating bronchioles, and redirecting blood flow to skeletal muscles. The parasympathetic nervous system, by contrast, promotes rest-and-digest functions, slowing the heart, stimulating digestion, and constricting the pupils. These two branches often exert opposing effects on the same target organs, and the balance between them determines the resting physiological state of the body.
The neurotransmitters that mediate autonomic signaling are acetylcholine and norepinephrine. Acetylcholine is the primary neurotransmitter at all autonomic ganglia and at parasympathetic postganglionic nerve endings, where it acts on cholinergic receptors. Norepinephrine is the primary neurotransmitter at most sympathetic postganglionic nerve endings, where it acts on adrenergic receptors. The rich pharmacology of these two neurotransmitter systems provides numerous targets for therapeutic intervention, making autonomic pharmacology one of the most clinically relevant areas of drug therapy.
Key Terms
The branch of pharmacology concerned with drugs that affect the autonomic nervous system, including both sympathetic and parasympathetic divisions.
The division of the ANS that mediates fight-or-flight responses through adrenergic neurotransmission.
The division of the ANS that promotes rest-and-digest functions through cholinergic neurotransmission.
A chemical messenger released at nerve terminals that transmits signals across synapses to target cells.