Introduction to Hypertension and Antihypertensive Therapy
Hypertension, defined as a sustained systolic blood pressure of 130 mmHg or greater or a diastolic blood pressure of 80 mmHg or greater according to current ACC/AHA guidelines, affects approximately one in three adults worldwide and is the single largest modifiable risk factor for cardiovascular disease, stroke, and chronic kidney disease. Hypertension treatment is therefore a central focus of clinical medicine, and antihypertensive drugs represent one of the most commonly prescribed drug categories globally.
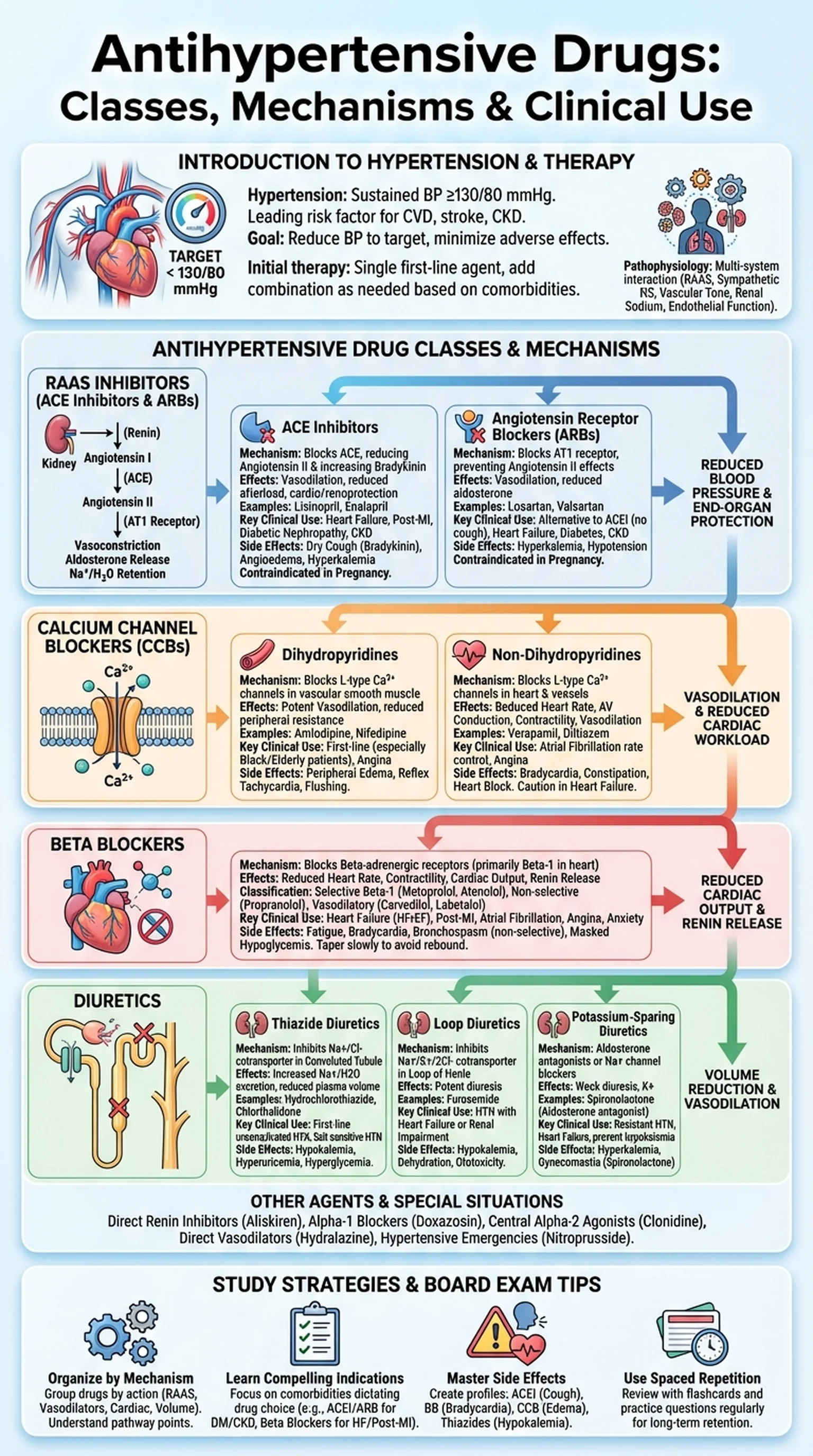
The pathophysiology of hypertension involves multiple interacting systems, including the renin-angiotensin-aldosterone system (RAAS), the sympathetic nervous system, vascular smooth muscle tone, renal sodium handling, and endothelial function. Antihypertensive drugs target these pathways at various points to lower blood pressure and reduce end-organ damage. The major classes of antihypertensive drugs include ACE inhibitors, angiotensin receptor blockers, calcium channel blockers, beta blockers, and diuretics, each with distinct mechanisms of action and clinical indications.
The goal of hypertension treatment is to reduce blood pressure to target levels while minimizing adverse effects and maximizing adherence. Current guidelines recommend a target of less than 130/80 mmHg for most adults with hypertension. Initial therapy typically involves a single first-line agent, with combination therapy added as needed to achieve blood pressure control. The choice of antihypertensive drug depends on the patient's age, race, comorbidities, and the presence of compelling indications such as heart failure, diabetes, or chronic kidney disease that favor certain drug classes over others.
Key Terms
Medications used to lower blood pressure and reduce the cardiovascular complications of hypertension, including ACE inhibitors, ARBs, CCBs, beta blockers, and diuretics.
A chronic condition defined by sustained elevated blood pressure (>=130/80 mmHg); the leading modifiable risk factor for cardiovascular disease.
A hormonal cascade that regulates blood pressure and fluid balance through angiotensin II and aldosterone; the target of ACE inhibitors and ARBs.
Damage to the heart, brain, kidneys, and vasculature caused by chronic uncontrolled hypertension.