Introduction to NSAIDs and Their Clinical Importance
Nonsteroidal anti-inflammatory drugs, universally known as NSAIDs, are among the most widely used medications in the world. Every year, billions of doses of NSAIDs are consumed globally for the relief of pain, inflammation, and fever. From over-the-counter staples like aspirin and ibuprofen to prescription-strength agents like indomethacin and ketorolac, NSAID types span a broad range of chemical structures, potencies, and clinical applications. Understanding the NSAID mechanism of action is fundamental to pharmacology education and clinical practice.
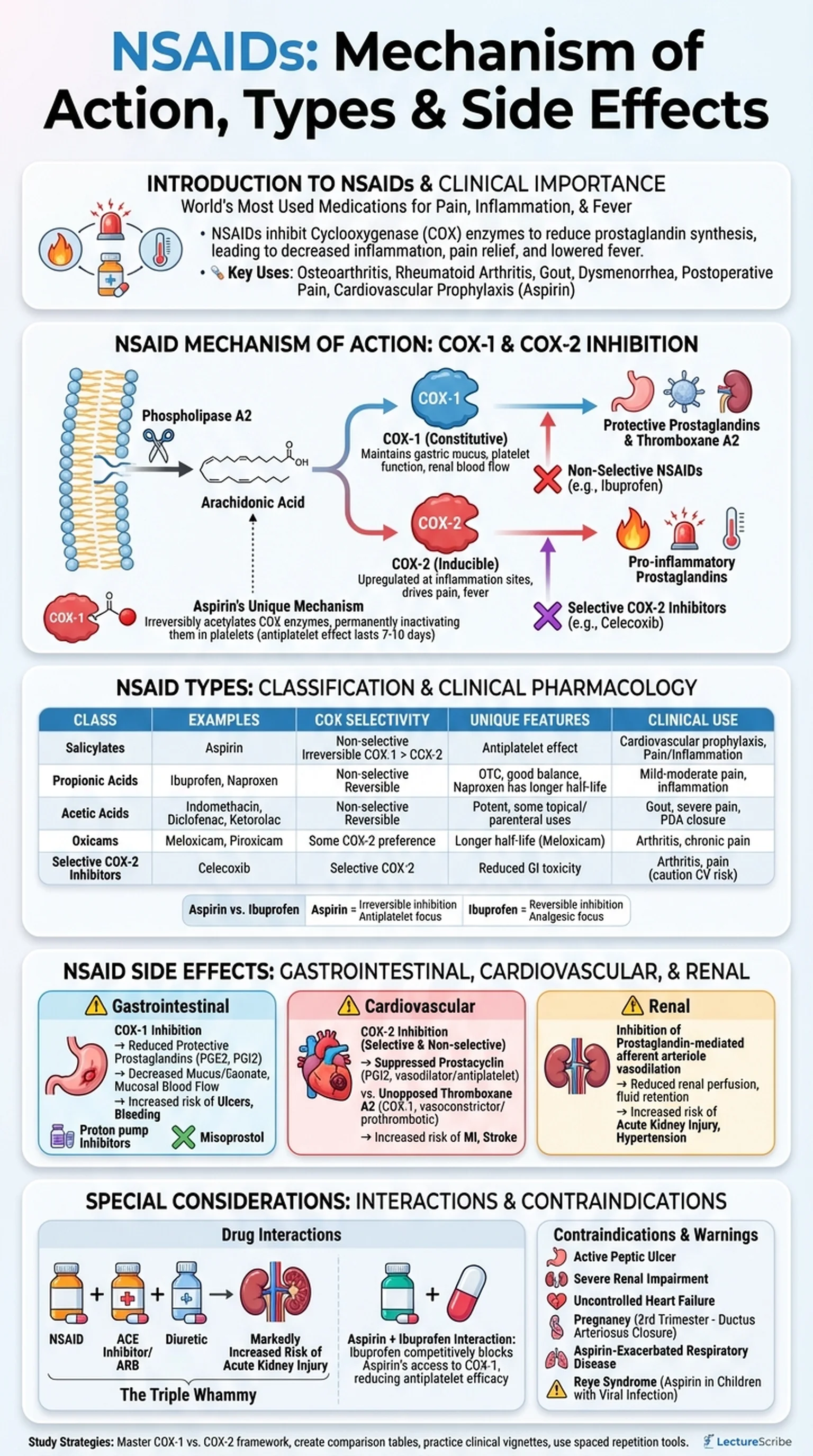
NSAIDs exert their effects by inhibiting cyclooxygenase (COX) enzymes, which catalyze the conversion of arachidonic acid into prostaglandins, thromboxanes, and prostacyclins. These lipid mediators play critical roles in inflammation, pain signaling, platelet aggregation, gastric mucosal protection, and renal blood flow regulation. By blocking COX activity, NSAIDs reduce the synthesis of pro-inflammatory prostaglandins, thereby decreasing inflammation, alleviating pain, and lowering fever.
The clinical importance of NSAIDs extends far beyond simple analgesia. These drugs are first-line therapy for conditions ranging from osteoarthritis and rheumatoid arthritis to dysmenorrhea, gout flares, and postoperative pain. Low-dose aspirin remains a cornerstone of cardiovascular prophylaxis due to its irreversible inhibition of platelet thromboxane A2 synthesis. However, the therapeutic benefits of NSAIDs must always be balanced against their potential for significant adverse effects, particularly gastrointestinal, cardiovascular, and renal toxicity. This balance between benefit and risk makes the study of NSAID side effects an essential component of pharmacological education.
Key Terms
Nonsteroidal anti-inflammatory drug; a class of medications that reduce inflammation, pain, and fever by inhibiting cyclooxygenase enzymes.
An enzyme that catalyzes the conversion of arachidonic acid to prostaglandins and thromboxanes; the primary molecular target of NSAIDs.
A lipid mediator derived from arachidonic acid that plays roles in inflammation, pain, fever, gastric protection, and renal function.
A 20-carbon polyunsaturated fatty acid released from cell membrane phospholipids; the precursor for prostaglandin and thromboxane synthesis.