Introduction to Blood Vessels and the Vascular System
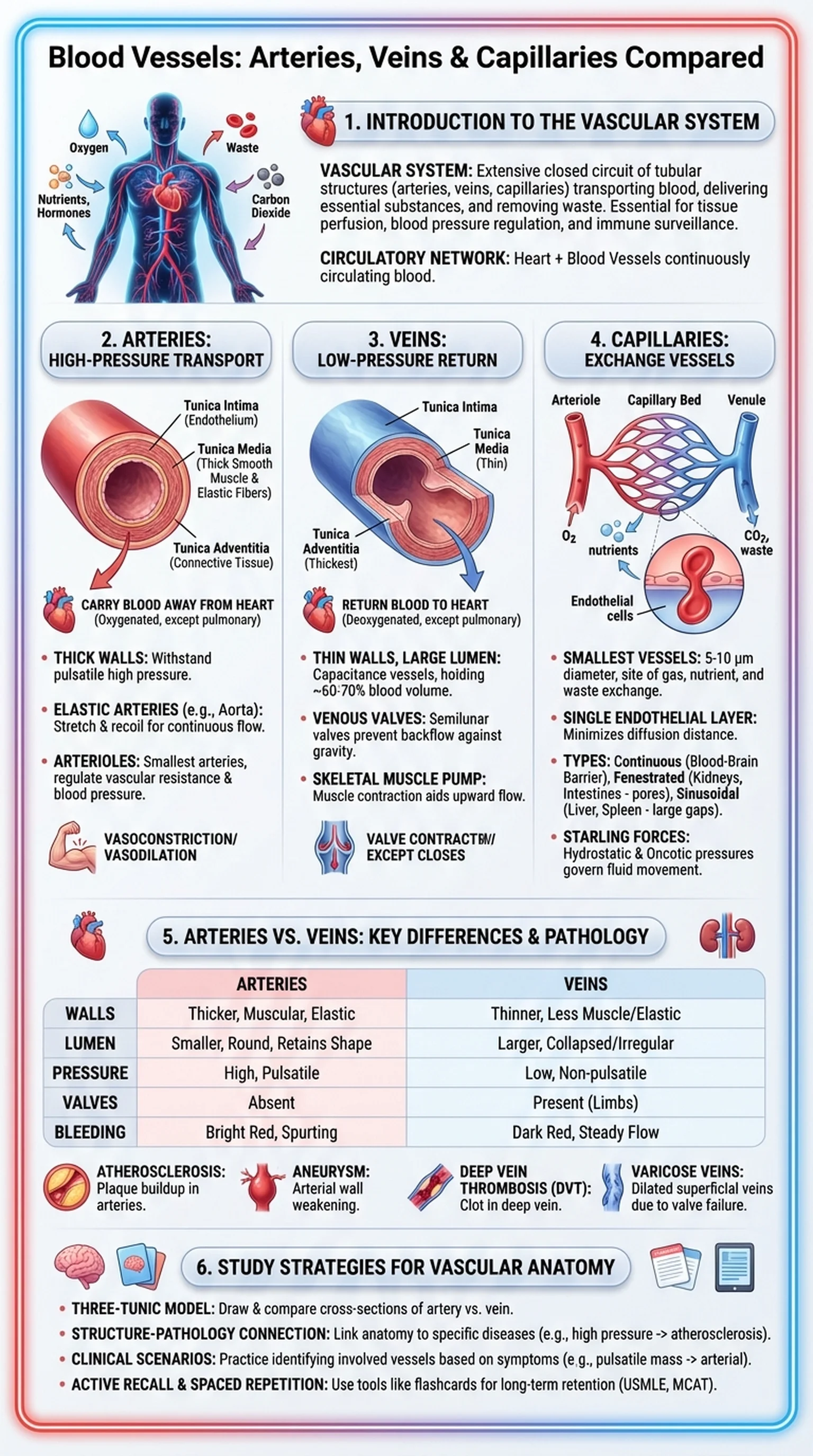
Blood vessels are the tubular structures that form the circulatory network responsible for transporting blood throughout the human body. Together, these vessels constitute the vascular system, an extensive closed circuit that delivers oxygen, nutrients, and hormones to tissues while removing metabolic waste products like carbon dioxide and urea. The vascular system is essential for maintaining tissue perfusion, regulating blood pressure, and enabling immune surveillance. Without a functioning network of blood vessels, no organ in the body could sustain its metabolic needs.
The vascular system is organized into three major categories of blood vessels: arteries, veins, and capillaries. Arteries carry oxygenated blood away from the heart to the tissues (with the exception of the pulmonary arteries, which carry deoxygenated blood to the lungs). Veins return deoxygenated blood from the tissues back to the heart (with the exception of the pulmonary veins). Capillaries are the microscopic vessels that connect the arterial and venous systems, forming the site where gas exchange, nutrient delivery, and waste removal actually occur.
Understanding blood vessels is foundational for students of anatomy, physiology, and clinical medicine. The structural differences between arteries, veins, and capillaries directly relate to their functional roles. Clinical conditions affecting blood vessels, including atherosclerosis, deep vein thrombosis, aneurysms, and varicose veins, are among the leading causes of morbidity and mortality worldwide. A strong grasp of vascular anatomy is therefore essential for diagnosing and managing cardiovascular disease.
Key Terms
Tubular structures including arteries, veins, and capillaries that form the circulatory network for transporting blood throughout the body.
The complete network of blood vessels in the body, including arteries, veins, and capillaries, responsible for circulating blood to all tissues.
The closed system of blood vessels and the heart that continuously circulates blood, delivering oxygen and nutrients while removing waste.
The passage of blood through the vascular system to an organ or tissue, ensuring adequate delivery of oxygen and nutrients.