What Is the Brachial Plexus?
The brachial plexus is one of the most clinically significant nerve networks in the human body. It is a complex arrangement of nerve fibers that originates from the spinal cord and provides motor and sensory innervation to the entire upper limb, including the shoulder, arm, forearm, and hand. Understanding brachial plexus anatomy is essential for medical students, physical therapists, and any healthcare professional who treats injuries of the upper extremity.
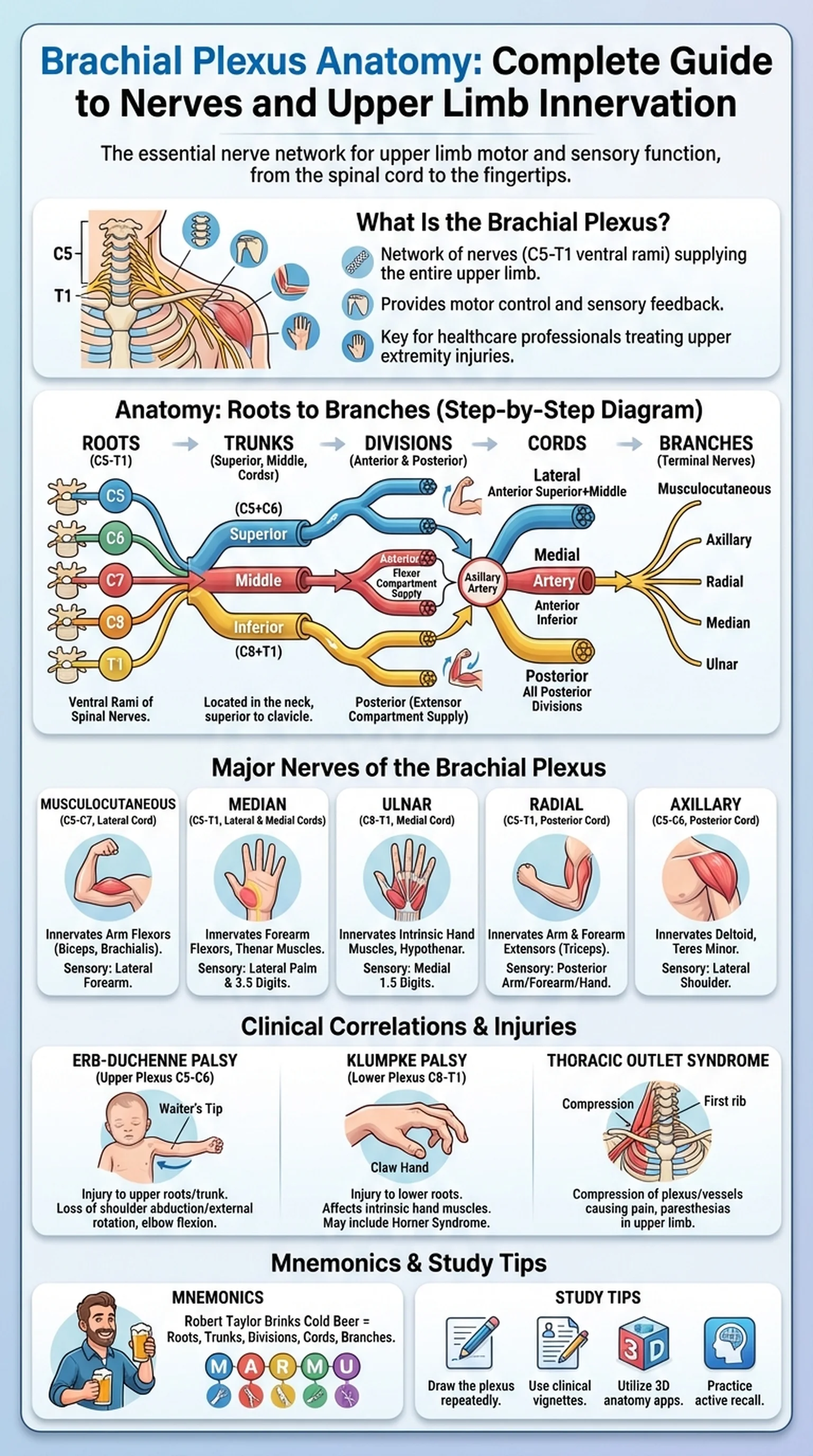
The brachial plexus is formed by the ventral rami of spinal nerves C5, C6, C7, C8, and T1. These nerve roots emerge from the intervertebral foramina of the cervical and upper thoracic spine and converge in the posterior triangle of the neck before passing into the axilla. The network undergoes a series of merging and branching events that ultimately produce the named peripheral nerves responsible for upper limb innervation. This intricate organization allows the nervous system to distribute fibers from multiple spinal levels to individual muscles and skin regions, providing redundancy and precise motor control.
Brachial plexus anatomy is a cornerstone of gross anatomy courses and appears frequently on examinations such as the USMLE, COMLEX, and NBME shelf exams. Clinicians encounter brachial plexus injuries in trauma settings, obstetric complications, and surgical procedures involving the neck and shoulder. A firm grasp of the plexus structure enables accurate localization of nerve lesions based on a patient's motor and sensory deficits. For these reasons, dedicating focused study time to the brachial plexus pays dividends throughout a medical career.
In the sections that follow, we will walk through each organizational level of the brachial plexus, identify the major brachial plexus nerves that arise from it, discuss clinical correlations and common injuries, and share proven mnemonics and study strategies to help you retain this material efficiently.
Key Terms
A network of nerves formed by the ventral rami of C5-T1 that provides motor and sensory innervation to the upper limb.
The anterior division of a spinal nerve that supplies the limbs and the anterolateral trunk.
The distribution of motor and sensory nerve fibers to the shoulder, arm, forearm, and hand via the brachial plexus.
An anatomical region bounded by the sternocleidomastoid, trapezius, and clavicle through which the brachial plexus passes.
Bundles of nerve fibers emerging from the spinal cord that combine to form the brachial plexus (C5-T1).