What Is Epithelial Tissue?
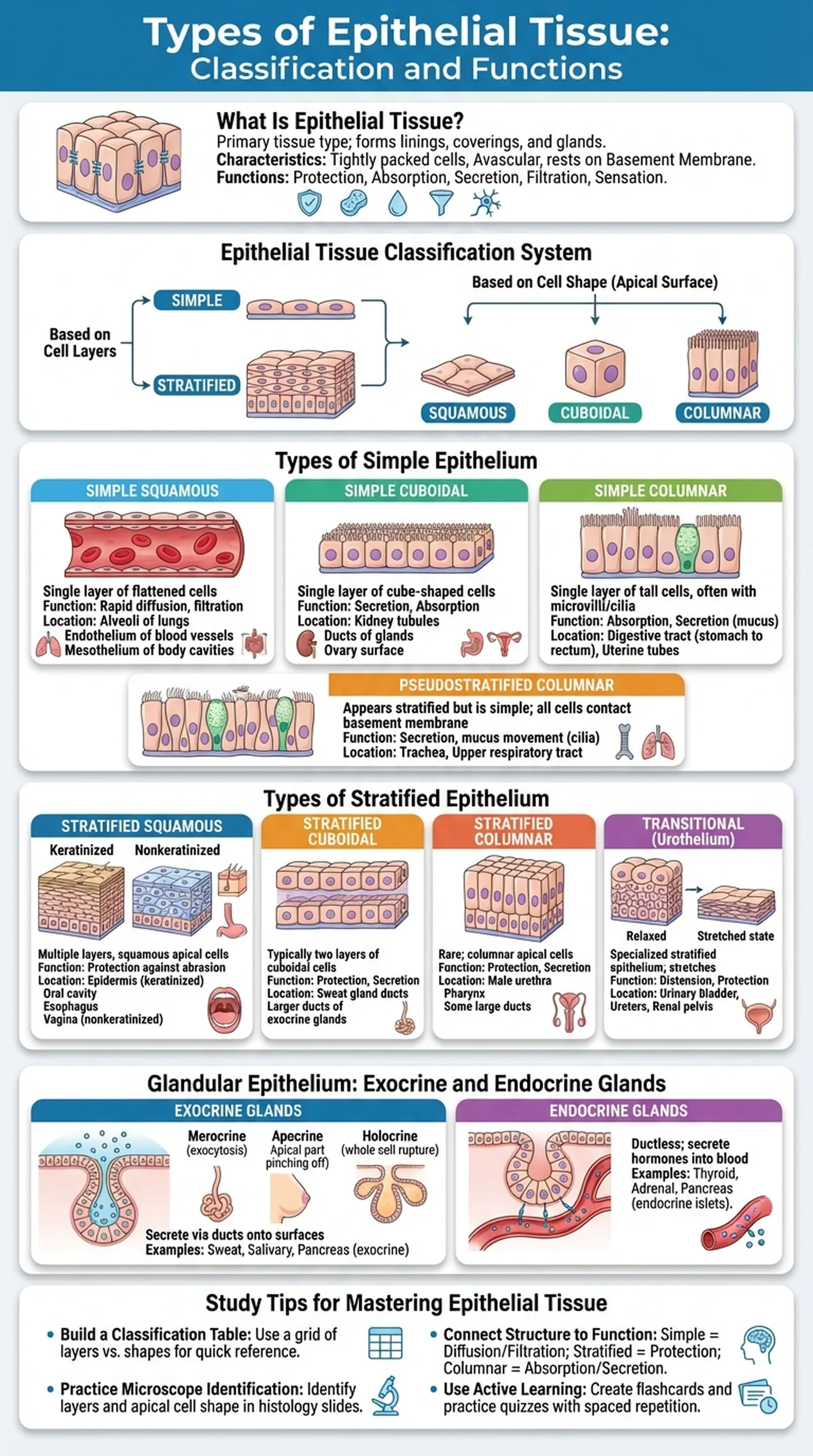
Epithelial tissue is one of the four primary tissue types in the human body, alongside connective, muscle, and nervous tissue. It forms the linings and coverings of virtually every body surface, from the skin that protects us from the external environment to the delicate lining of the small intestine that absorbs nutrients. Understanding epithelial tissue is fundamental for students of anatomy, histology, pathology, and medicine because alterations in epithelial cells are at the root of many diseases, including the vast majority of human cancers (carcinomas).
All types of epithelium share several defining characteristics. First, epithelial cells are tightly packed with minimal extracellular matrix between them, connected by specialized junctions such as tight junctions, adherens junctions, desmosomes, and gap junctions. Second, epithelial tissue is avascular, meaning it lacks its own blood supply and must receive nutrients by diffusion from the underlying connective tissue. Third, all epithelial tissue rests on a basement membrane, a thin extracellular layer composed of a basal lamina and a reticular lamina that anchors the epithelium to the connective tissue below.
Epithelial tissue performs a wide range of functions depending on its location: protection against mechanical abrasion, pathogens, and chemical damage; absorption of nutrients and ions; secretion of mucus, hormones, and enzymes; filtration of blood in the kidneys; and sensation through specialized neuroepithelial cells. The epithelial tissue classification system organizes these diverse tissues based on two criteria: the number of cell layers and the shape of the cells at the free (apical) surface. This dual classification scheme produces the major types of epithelium that every anatomy student must master.
Key Terms
One of the four primary body tissues, characterized by tightly packed cells that line body surfaces, cavities, and glands, resting on a basement membrane.
A thin extracellular layer composed of a basal lamina and reticular lamina that anchors epithelial tissue to the underlying connective tissue.
Cell junctions that form a seal between adjacent epithelial cells, preventing the passage of molecules through the intercellular space.
Lacking blood vessels; epithelial tissue receives nutrients by diffusion from capillaries in the underlying connective tissue.
A malignant tumor arising from epithelial tissue, representing the most common category of cancer in humans.