Overview of the Respiratory System
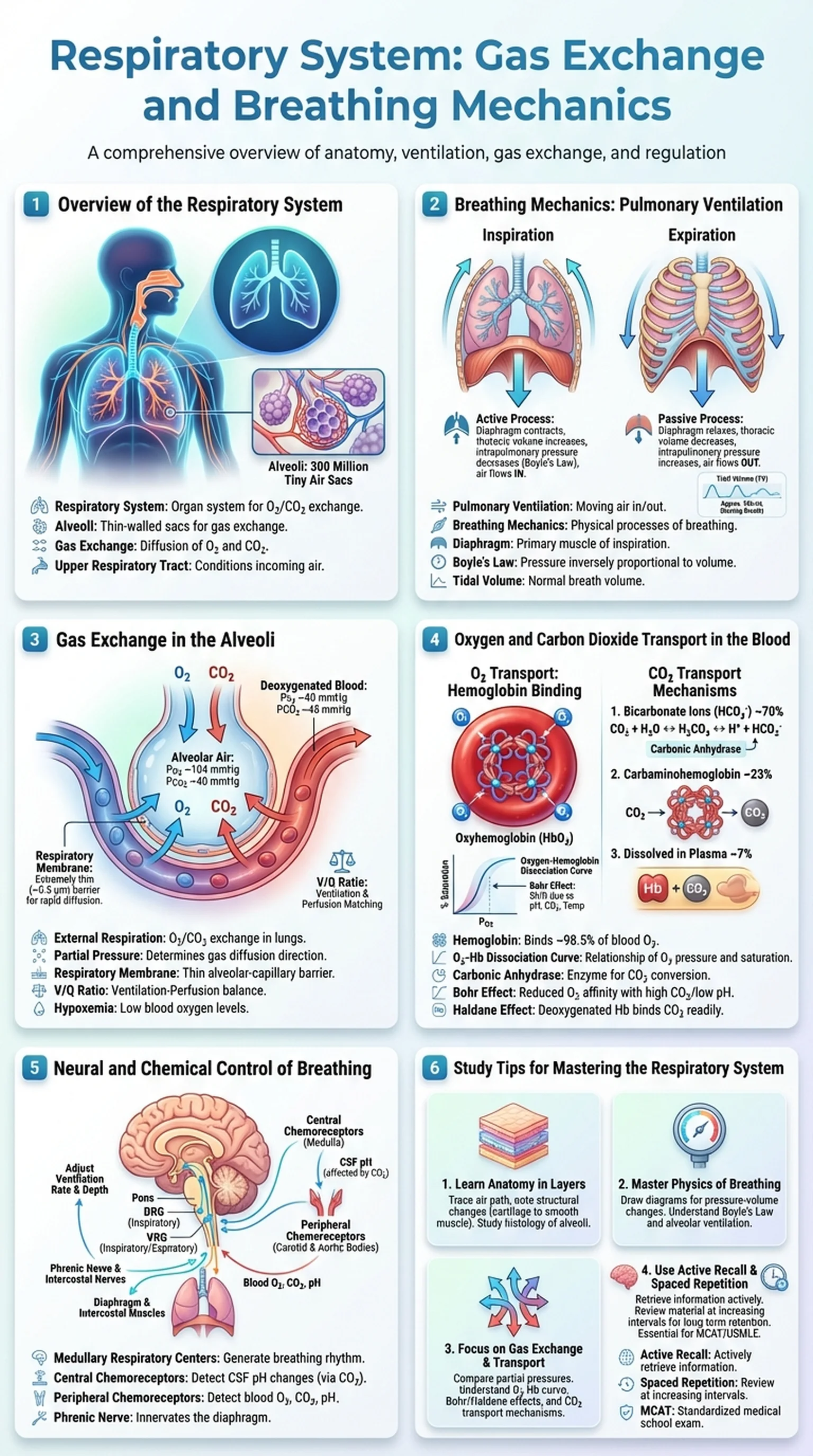
The respiratory system is the organ system responsible for the exchange of gases between the body and the external environment. Its primary function is to deliver oxygen to the blood and remove carbon dioxide, a metabolic waste product, from the body. The respiratory system works in close partnership with the cardiovascular system to ensure that every cell in the body receives the oxygen it needs for aerobic metabolism and that carbon dioxide is efficiently eliminated.
Anatomically, the respiratory system is divided into the upper respiratory tract and the lower respiratory tract. The upper respiratory tract includes the nose, nasal cavity, pharynx, and larynx. These structures warm, humidify, and filter the incoming air before it reaches the lungs. The lower respiratory tract includes the trachea, bronchi, bronchioles, and lungs, where the actual process of gas exchange occurs. The lungs contain approximately 300 million alveoli, tiny air sacs with extremely thin walls that provide an enormous surface area (approximately 70 square meters) for the diffusion of oxygen and carbon dioxide.
Understanding the respiratory system is essential for students of anatomy, physiology, and medicine. Respiratory diseases, including asthma, chronic obstructive pulmonary disease (COPD), pneumonia, and pulmonary embolism, are among the leading causes of morbidity and mortality worldwide. A solid grasp of respiratory anatomy, breathing mechanics, and the principles of gas exchange enables students to understand how these diseases disrupt normal function and how treatments work to restore it. In this article, we will explore the anatomy of the respiratory system, the mechanics of pulmonary ventilation, the process of gas exchange in the alveoli, and the transport of oxygen and carbon dioxide in the blood.
Key Terms
The organ system responsible for gas exchange, delivering oxygen to the blood and removing carbon dioxide from the body.
Tiny, thin-walled air sacs in the lungs where gas exchange between air and blood occurs across the respiratory membrane.
The diffusion of oxygen from the alveoli into the pulmonary capillaries and carbon dioxide from the capillaries into the alveoli.
The portion of the respiratory system that includes the nose, nasal cavity, pharynx, and larynx, which condition incoming air.